Navatar Health is transforming how patients are engaged, educated, and guided to take action—starting with colorectal cancer screening and expanding across the healthcare journey. Our insight is simple but powerful: in healthcare, knowing is not doing. Behavior is the missing link between medical knowledge and real-world outcomes.
Every year, tens of thousands of Americans die from cancers we know how to prevent. Screening is available, covered, and recommended—but nearly one-third of eligible people remain unscreened. Mailing test kits and sending reminders isn’t enough.
The real barriers are emotional: fear, confusion, cultural disconnect, and mistrust. And in a fee-for-service system under constant time pressure, most patients don’t get the support they need to overcome them.
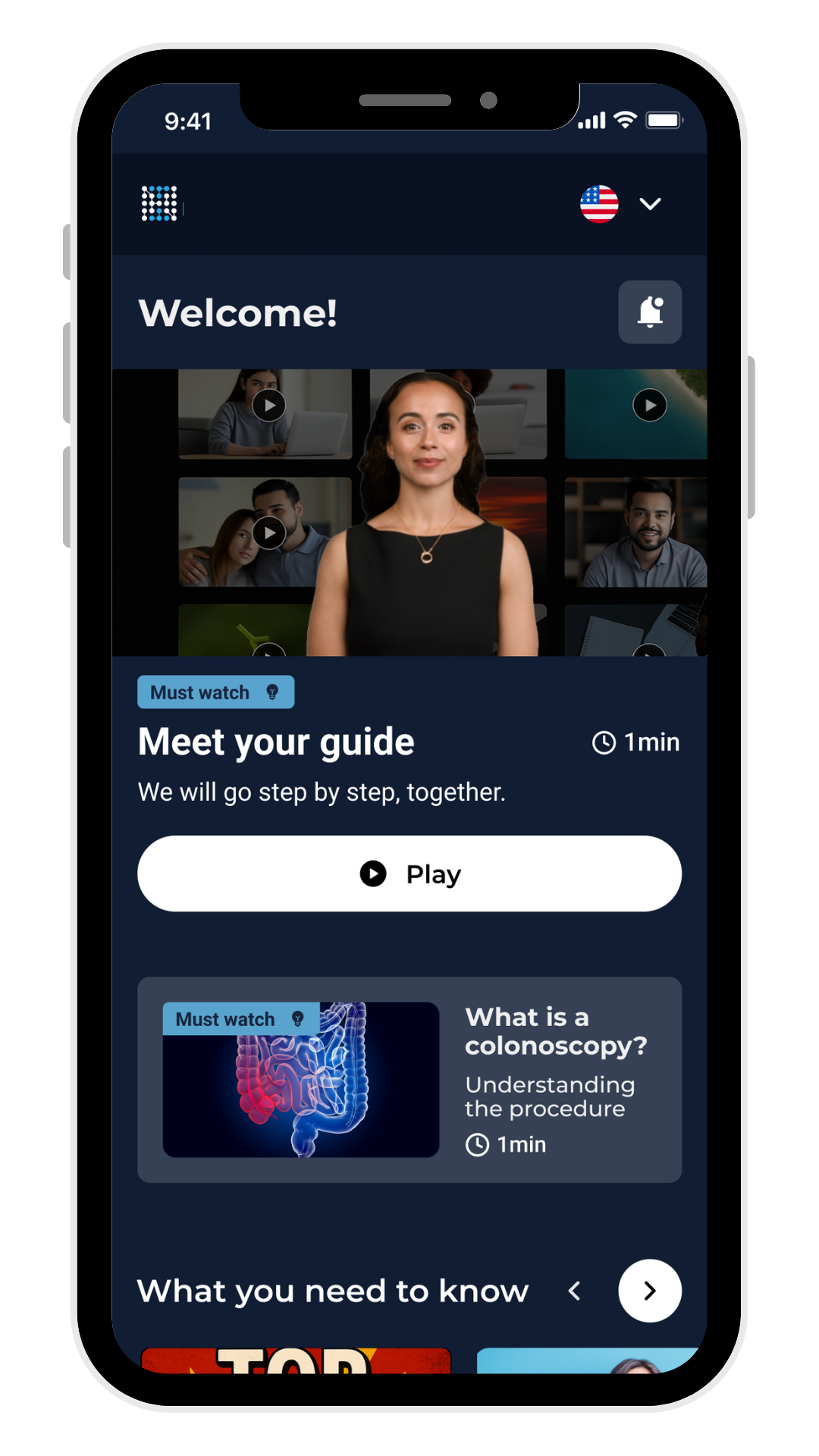
Navatar Health was built to change that. Our platform uses AI-generated nurse-navigator avatars—called Navatars—to deliver emotionally intelligent, culturally tailored, behaviorally optimized engagement. Patients choose the language and identity that best reflects them, and the platform adapts to provide clear, persuasive, respectful guidance.
Navatar meets people where they are—emotionally, linguistically, and culturally—and helps move them from intention to action.
At Navatar Health, we believe that true transformation in healthcare begins not just with better information—but with a deeper understanding of how people learn, decide, and act. Health decisions are rarely made through logic alone. They are shaped by emotion, identity, social norms, trust, and the subtle forces of habit and context.
Too often, patients are expected to navigate complex medical choices with limited support, low-quality communication, or messages that fail to resonate. Language barriers, low health literacy, and cultural disconnects create serious knowledge gaps. But even when people do understand the facts, they may still struggle to act.
That’s why Navatar doesn’t stop at information. We design for behavior—honoring the reality that people don’t always think what they feel, say what they think, or do what they say. We meet people where they are, using behavioral science, emotionally intelligent storytelling, and AI-powered personalization to guide them toward better choices. We’re building tools that connect not just with the mind, but with the human experience—because healthcare doesn’t change until people do.
Our mission is to turn knowledge into action and prevention into possibility. We empower people to make better health decisions—starting with those at risk for colorectal cancer—by delivering digital tools that engage, educate, motivate, and guide. Navatar serves as a trusted, culturally tailored navigation layer across the healthcare journey, helping patients move from confusion to clarity, and from intention to action.

Dr. David Perdue is a visionary healthcare leader, board-certified gastroenterologist, and health technology innovator. An enrolled member of the Chickasaw Nation, Dr. Perdue brings over two decades of experience in clinical care, preventive oncology research, and quality improvement. He is the Founder and Principal of Navatar Health, a digital health company focused on using AI-powered technologies to enhance patient engagement, streamline care delivery, and improve health outcomes. His work combines clinical expertise with cutting-edge technology to close gaps in care, address disparities, and make preventive healthcare more accessible and effective.Before launching Navatar Health,
Dr. Perdue held several senior leadership roles, including Chief Medical Officer and Board Member at MNGI Digestive Health, one of the largest private gastroenterology practices in the U.S. In these positions, he led enterprise-wide initiatives to optimize care quality, operational efficiency, and patient experience. He developed scalable programs to enhance clinical documentation, streamline workflows, and deliver exceptional care. Dr. Perdue also has a strong academic foundation, having served as a faculty member at the University of Minnesota, and Founder and Medical Director for the American Indian Cancer Foundation, where he advanced cancer prevention research and initiatives.Dr. Perdue’s vision is to redefine how healthcare leverages technology to improve lives.
With a career rooted in addressing barriers to care and improving cancer prevention, he is now focused on scaling AI-driven solutions to empower patients and providers. His academic and professional background—including a Master’s in Public Health, postdoctoral training in cancer research, and Chief Quality Officer certification—reflects his deep commitment to evidence-based innovation. As a healthcare entrepreneur, Dr. Perdue is dedicated to building scalable, data-driven solutions that make care more personalized, efficient, and impactful.